In my dermatology practice, I get all sorts of questions, from why hormonal acne is flaring up to if it’s “normal” to have a certain rash.
Sometimes, I get the fearful query, “is this melanoma?”
I’ve seen many patients beat this disease, and I want to take the fear of the unknown out of the equation. Let’s break down symptoms, causes, types of melanoma, and treatment together.
As the saying goes, “knowledge is power.” When a new mole pops up, do you know what to do, or better yet, how to prevent possible melanoma cells?
The National Cancer Institute states that early detection is key to beating this skin cancer battle, so let’s take a closer look.
What is Melanoma?
Melanoma is a type of skin cancer and begins as cells called melanocytes. It is also called cutaneous melanoma or malignant melanoma.

While it makes up less than 1% of skin cancer cases, it is among the most serious (when compared to basal cell carcinoma (BCC) and squamous cell carcinoma (SCC)). It’s considered dangerous because it is known to spread quickly throughout the body if not diagnosed early.
Why is melanoma so deadly? Melanoma is so deadly because if allowed to spread, the cancer cells can infect the lymphatic system and even into bone and organs. However, when caught early, the survival rate is quite high.
Melanoma affects skin cells known as melanocytes. These cells produce pigment, or melanin, in the skin, and are responsible for things like freckles and moles. When melanocytes become cancerous, pre-existing or new moles begin to form tumors. Read on to learn how to spot them.
Melanoma Symptoms
What do early signs of melanoma look like? Early signs of melanoma can be boiled down to a few common characteristics in a mole.
These early signs can be broken down into the acronym ABCDE.
It’s time to get a mole checked if you notice irregularities in its:
- Asymmetry: if the mole is not the same shape on both halves
- Border: if the edges of the mole are blurry or irregular
- Color: if the mole is colored unevenly or has patches of different colors
- Diameter: if the mole is growing in size
- Evolution: if the mole has changed, or continues to change
If you see any of these irregularities or have any questions about moles or spots on your skin, it’s time to head to your dermatologist for a follow-up.
Moles that are unusual in size, shape, or color can be referred to as “dysplastic nevi” or “atypical nevi”. These changes may happen with both new moles or previously normal moles, so check your skin regularly. You may also notice bleeding or itching.
How long do you live after being diagnosed with melanoma? You can live a very long life even after a melanoma diagnosis, especially if caught quickly.
If melanoma is diagnosed at an early stage before it spreads, it carries a 99% survival rate. That figure drops to 65% once melanoma has entered the lymph nodes, and 25% once it infiltrates the organs.
Hidden Melanomas
Most of us think of melanoma as a cancerous lesion that appears on the visible portions of the skin. However, this skin cancer can develop on any surface of the skin that includes pigment.

Unfortunately, this means that it’s possible for “hidden melanomas” to develop in unseen and/or unexpected places.
Hidden melanomas may occur on:
- Fingernail and/or toenail beds (under the nail)
- The palms of your hands
- The soles of your feet
- The mouth
- The digestive tract (mouth, esophagus, or anus)
- The urinary tract
- The vagina
- The uvea (the space under the whites of your eyes)
These are rare types of melanomas, known as:
- Acral lentiginous melanoma (nail beds, hands, and feet)
- Mucosal melanoma (mouth, digestive tract, urinary tract, or vagina)
- Ocular melanoma (eyes)
Sadly, mucosal melanoma is often misdiagnosed or overlooked entirely, as it often presents as another condition.
Causes of Melanoma
Typically, the body grows new layers of skin cells that push the older cells to the surface. However, when the DNA of melanocytes becomes damaged and the repair mechanisms don’t work, it can cause an overgrowth of new skin cells. These can compound into a tumor.
While no one is certain why the DNA of certain skin cells is harmed and repair mechanisms fail, science points to an unfortunate combination of factors from a person’s genetics and environmental factors.
Melanoma Risk Factors
Risk factors associated with developing melanoma include:
- Frequent sunburns: If you stay out in the sun for long periods of time and develop sunburns, the damage to your skin cells may contribute to the development of skin cancer. That’s one major reason it’s so important to use sun protection anytime you sunbathe or are outdoors for prolonged period of time.
- Your race. The American Cancer Society found that white people are the most likely to develop skin cancer (at a lifetime risk of 2.6%), followed by 0.6% for Hispanic people, and 0.1% for black people. That’s right, Caucasians are 20 times more likely to develop this cancer. The more fair-skinned you are, the higher your risk. However, most of us are a blend of multiple races so it’s challenging to apply some of these statistics to real life. The bottom line is that all races can get skin cancer.
- UV exposure: When it comes to environmental factors, ultraviolet rays, or UV radiation, seem to be the main offenders. These can penetrate the skin naturally through sunlight, tanning beds, UV lamps, and even some welding equipmentThe windshield and windows of your car and even your home also don’t fully protect you even if they are tinted and this is the most common way you can get substantial hidden UV exposure without realizing it.
- Tanning beds: One tanning bed session, yes ONE session, increases your risk for melanoma by 20%, squamous cell carcinoma by 67% and basal cell carcinoma by 29%. If you used a tanning bed before the age of 30 and you are female, you are 6 times more likely to develop melanoma.
- Living near the equator and/or at high elevations: These locations bring you physically closer to the sun, which is probably why they’re known risk factors for melanoma.
- Presence of moles: When you have more than 50 regular moles or any irregular moles (dysplastic nevi), your chances of developing melanoma are higher.
- Impaired immune system: If your immune system is weak or compromised, your body may not be as able to fight off the abnormal cell development that turns into skin cancers. This includes people with chronic health conditions, autoimmune issues, have undergone chemotherapy, or are undergoing any medical treatments that suppress the immune system.
- Genetics: If you have a family history of melanoma, it’s more likely that you may end up with the condition, too.
Additionally, not all places in the body are equally likely to develop melanoma. While it’s possible to develop this cancer anywhere on the body that has pigment, such as in the intestines or eyes (ocular melanoma), it’s far more likely to develop in places that have frequent sun exposure.

These places include:
- The neck for both men and women
- The face for both men and women
- The legs for women
- The chest and back for men
Types of Melanoma
This discussion likely has you wondering: What are the 4 types of melanoma? The 4 types of melanoma are superficial spreading, nodular, lentigo maligna, and acral lentiginous. Each of these 4 has distinct characteristics.
1. Superficial Spreading
This is the most common type of melanoma, spreading primarily across the surface of the skin. This variation is characterized by moles with irregular borders and uneven coloring.
2. Nodular
Nodular melanoma spreads more deeply into the layers of the skin. It often presents as a bump or lump underneath a raised mole.
3. Lentigo Maligna
This type of melanoma is common on parts of the body that receive more sun exposure. It typically develops with age and can present as an uneven, dark pigmented patch across a larger portion of skin.
4. Acral Lentiginous
Acral lentiginous melanoma originates in locations that may surprise you: the soles of the feet, palms of the hands, or under the nail beds.
This type of melanoma is more common in people of color and those of Asian descent.
Where does melanoma usually spread to first? Melanoma first spreads to the lymph nodes. Once melanoma has passed the basement membrane of the skin and entered internal systems, it typically heads to the nearest lymph node.
Prevention
One of the best things you can do for your skin is to take good care of it with practices like:
- Wearing sun protection.. Long-sleeves, long pants, wide-brimmed hat, sunglasses and sunscreen where you can’t cover with clothes is our top recommendation. Sun Protection helps prevent sunburns, which damage melanocytes, and also block ultraviolet light, which may cause melanoma. Try to use zinc oxide based sunscreen with an SPF of at least 30 and reapply after strenuous activities or two hours, whichever comes first.
- Avoiding direct sunlight during the middle of the day. The ultraviolet rays of the sun are generally strongest during this time. Depending on your climate, the time of strongest rays may vary. Here in Arizona during the hot summers, most of us try to get outdoor things done before sunrise or after sunset as the sun is very powerful all day long. But for the most part, try to limit or stay out of the sun between 10am and 4 PM.
- Covering up. If you are outside during these hours, try wearing protective clothing like a hat and long sleeves.
- Wearing eye protection. This protects the melanocytes in your eyes from UV rays.
- Supporting your immune system. Your body is better able to defend against cancer or sustain treatments if it’s properly cared for.
Melanoma Diagnosis & Treatment
When a doctor or dermatologist suspects melanoma in a mole, they will take a skin biopsy of the lesions in question to determine whether or not they are cancerous. This is the only conclusive way to determine if the mole is cancerous or a nonmelanoma.
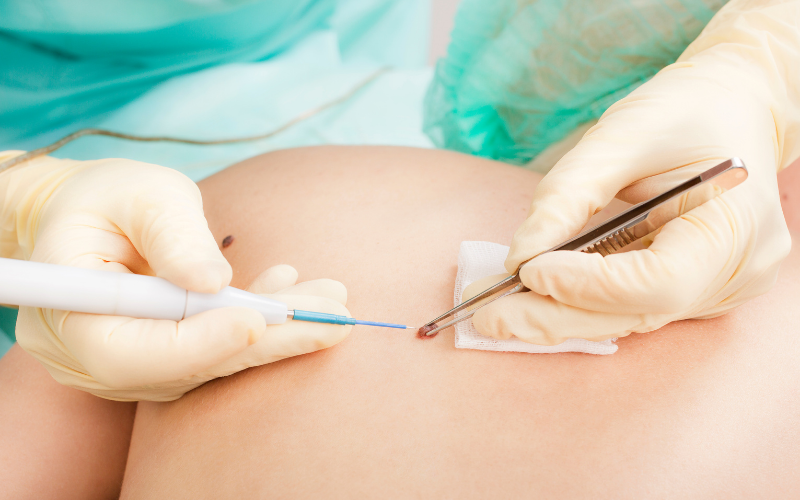
If needed, they may also recommend that you have a biopsy of a nearby lymph node, or perform a CT scan, MRI, or PET scan. Once they’ve determined the cancer’s stage, they can determine the best treatment option.
Once any type of melanoma has spread past the epidermis into the lymph nodes or surrounding tissues, it is referred to as metastatic melanoma.
If you have a later stage case, you will likely need additional treatment options, which might include immunotherapy drugs, targeted therapy for cancers related to BRAF or C-Kit genes, chemotherapy, or radiation.
When to See a Doctor/Dermatologist
Ideally, you will be performing regular self-examinations of your moles. It’s a good time to see a doctor or dermatologist as soon as you notice a mole that is concerning. Ask your doctor to perform a skin check if they don’t already do it during your annual exam.
After visiting the doctor, it may turn out that the spot you were concerned about may also be a squamous cell carcinoma (SCC) or basal cell carcinoma (BCC), so it’s certainly worth checking out any confusing spot on your skin for your own peace of mind. Even if it is something, early detection gives you a great start on treating your melanoma.
If you’ve just been diagnosed with melanoma, I’ve created a quick and simple guide to what to expect and how to talk to your dermatologist about comprehensive treatment options.
 Diagnosed with melanoma? Here’s what to do next. Click here to get your FREE Melanoma Guide now.
Diagnosed with melanoma? Here’s what to do next. Click here to get your FREE Melanoma Guide now.
Remember, when melanoma is diagnosed early in the disease, the survival rate is very high! Don’t skip dermatology appointments and self-checks — and don’t forget to wear your sunscreen.
Sources
- Heistein, J. B., & Acharya, U. (2019). Cancer, Malignant Melanoma. In StatPearls [Internet]. StatPearls Publishing. Full text: https://www.ncbi.nlm.nih.gov/books/NBK470409/
- Ward, W. H., Lambreton, F., Goel, N., Jian, Q. Y., & Farma, J. M. (2017). Clinical presentation and staging of melanoma. Exon Publications, 79-89. Full text: https://www.ncbi.nlm.nih.gov/books/NBK481857/#:~:text=Developed%20for%20both%20physicians%20and,timing%20of%20the%20lesion’s%20growth.
- Puckett, Y., Wilson, A. M., & Thevenin, C. (2017). Cancer, Melanoma Pathology. Full text: https://www.ncbi.nlm.nih.gov/books/NBK459367/#:~:text=There%20are%20various%20types%20of,%2C%20common%20in%20African%20Americans).
- Domingues, B., Lopes, J. M., Soares, P., & Pópulo, H. (2018). Melanoma treatment in review. ImmunoTargets and therapy, 7, 35. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5995433/#:~:text=Depending%20on%20the%20features%20of,surgery%20is%20the%20primary%20treatment.
