What is Inflammaging?
Inflammaging is chronic low-grade inflammation associated with the aging process.
Sometimes described as smoldering inflammation or inflamm-aging, this is an inflammation that doesn’t go away after regular inflammatory responses do their job in the body.
The term “inflammaging” was coined by Italian researcher Claudio Franceschi in 2000 to describe our cell receptors’ inability to cope with attacks at the molecular level as we age.
Typically, inflammatory responses occur when your body is fighting off an infection or responding to external stressors. Those are good things! You want your body’s immune cells to do what they need to in order to fight pathogens and ward off illness.
With inflammaging, the body’s innate immune system is working in overdrive, behaving with an activated inflammatory response where one shouldn’t exist. The result is a higher risk of chronic diseases and literally aging faster.
Let’s take a closer look at the causes of this condition and what you can do about it for optimal health, even as you get older.
What Causes Inflammaging?
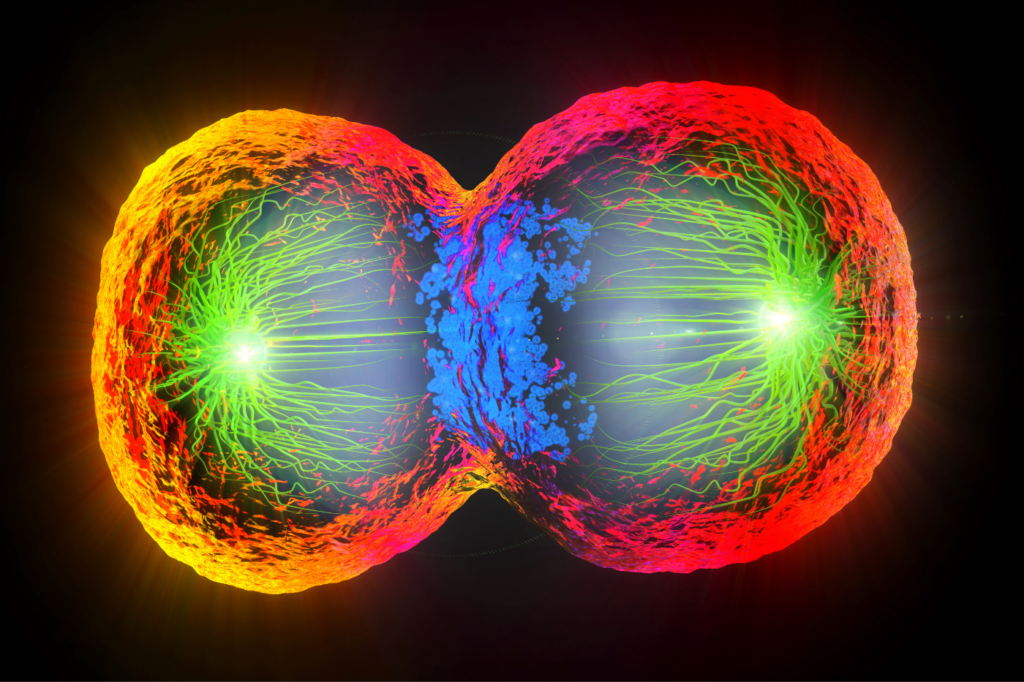
Inflammaging is caused by several mechanisms in the body that link back to human aging. As researchers look to identify inflammatory biomarkers, one of the primary causes appears to be cellular senescence.
Senescent cells are cells that permanently stop dividing, but don’t die. Instead, they remain in the body, triggering pro-inflammatory cytokines as a response.
This dysregulation and a lack of cell mediators can keep your body’s cytokines from the vital work of telling your immune and leukocyte cells what to do and where to go.
While the activation of these cells is essential in processes like wound healing, a natural inflammatory response, they can accumulate as we age. This can lead to an imbalance of homeostasis, harming nearby cells important to overall health.
The result can be difficulty fighting off illness and regulating oxidative stress, accelerating your risk of developing many age-related conditions and infections.
What is the difference between inflammaging and aging? The difference between inflammaging and aging is that while inflammaging is closely linked with the aging process, it does not occur in the same way in every elderly individual.
Inflammaging can be worse in those struggling with obesity, particularly with extra belly weight, and those struggling with chronic infections.
Unhealthy lifestyles, an imbalance of amino acids and gut microbiota (everything living in your digestive tract), and chronic stress can also contribute to inflammaging.
Why is Inflammaging Bad?
Inflammaging is bad because of the links experts continue to find between this cellular response and a host of chronic conditions and weakened immune responses.
It is often found in adverse health outcomes in the elderly, as many age-related illnesses have inflammatory origins. In fact, inflammation is a prominent part of the pathologies of many diseases.
These age-related illnesses include cardiovascular disease, atherosclerosis, autoimmune diseases, cancers, osteoporosis, and rheumatoid arthritis (an auto-inflammatory condition).
Inflammaging has also been linked to mental health conditions like depression as well as neuroinflammation associated with Alzheimer’s disease and related dementia.
When it comes to the skin, inflammaging can cause tissue damage, chronic skin conditions, collagen loss, and difficulties fighting skin infections.
This is on top of the decline of mitochondrial function as we age (a component of age-related conditions and skin aging) and hormone-related changes in the skin.
How Can I Reduce Inflammation?
You can reduce inflammation in several ways, such as getting regular exercise, eating a healthy diet, and managing stress.
These anti-inflammaging interventions cannot cure aging, but they can improve conditions common in advancing age, potentially slowing down the inflammaging process.
Keep in mind that while anti-inflammatory drugs can improve any pain associated with inflammation, they won’t address the underlying causes of your condition.
1. Get Regular Exercise
Regular exercise is essential to maintain a high quality of life as you age. It’s also an important factor in the fight against chronic inflammation and age-related diseases.
It is never too late to start a regular exercise regimen to reduce risk factors associated with a sedentary lifestyle.
New to exercise? Keep it simple. Taking a brisk daily walk in your own neighborhood is an excellent way to start and get you on track toward a healthier lifestyle.
2. Eat a Healthy Diet
The number of centenarians in European countries like Italy and Greece makes up a growing portion of the populations there.
Scientists studying aging and immunology have spent quite a bit of time looking at what accounts for an extended lifespan in what are known as the “Blue Zones.” The answer often lies in healthier dietary choices.
Following a Mediterranean diet focused on whole grains, fruits, vegetables, and healthy fats has been linked to a modulation of inflammation. Reducing your risk or even improving your symptoms can be as simple as improving your diet.
3. Avoid Inflammatory Triggers
When working to reduce inflammatory responses in the body, it’s crucial that you know the different types of triggers for inflammation.
The following foods can trigger inflammation or make existing inflammation worse:
- Red meats
- Processed meats, like sausages and lunch meat
- Fried foods
- Saturated/trans fats
- Drinks with added sugar, like sodas and some fruit juices
- High fructose corn syrup
- Refined carbohydrates, like white bread and sweet desserts
- Margarine/shortening
4. Consume Anti-Inflammatory Foods & Drinks
Boosting your consumption of foods known to fight inflammation can be just as important as ditching the triggers.
Unsurprisingly, these are foods found in the typical healthy diet, something you already know is a key component to overall health.
Foods that fight inflammation include:
-
- Olive oil
- Leafy green vegetables, like spinach and kale
- Nuts, like almonds and walnuts
- A variety of fruits, but especially berries
- Fatty fish, like salmon and mackerel
- Tomatoes
- Green tea
- Turmeric
5. Reduce Chronic Stress
Stress can not only make existing inflammation worse, but it can also trigger an inflammatory response in the body. When you’re feeling stressed, your body works to get you through that stressor by temporarily suspending your normal innate immunity functions.
Chronic stress can decrease your access to lymphocytes in the body. Lymphocytes are the white blood cells that keep your immune system strong, and reduced access to these cells puts you at risk for illness.
Regular exercise, yoga, meditation, or even identifying and removing significant stressors in your life can all help reduce chronic stress.
6. Get Better Sleep
Sleep is restorative. As we sleep, our body is allowed to reset, improving everything from the quality of your skin to brain function.
Even in healthy individuals, sleep loss is associated with inflammatory responses and metabolic dysfunction (leading to conditions like heart disease and type 2 diabetes).
That’s why it’s essential to stick with a regular sleep schedule. Pay attention to your body clock and work to improve your sleep. Go to bed and wake up around the same time every day. Limit screen time, caffeine, and other stimuli in the hours leading up to bed.
Consider melatonin if you find that your body isn’t creating enough on its own to manage your circadian rhythms. Invest in yourself and a relaxing bedtime routine to fight inflammation long-term.
Sources
- Franceschi C., Bonafè, M., Valensin, S., Olivieri F., De Luca, M., Ottaviani, E., & De Benedictis, G. (2000). Inflamm-aging. An evolutionary perspective on immunosenescence. Annals of the New York Academy of Sciences, 908, 244–254. Abstract: https://pubmed.ncbi.nlm.nih.gov/10911963/
- Furman, D., Campisi, J., Verdin, E., Carrera-Bastos, P., Targ, S., Franceschi, C., Ferrucci, L., Gilroy, D. W., Fasano, A., Miller, G. W., Miller, A. H., Mantovani, A., Weyand, C. M., Barzilai, N., Goronzy, J. J., Rando, T. A., Effros, R. B., Lucia, A., Kleinstreuer, N., & Slavich, G. M. (2019). Chronic inflammation in the etiology of disease across the life span. Nature medicine, 25(12), 1822–1832. Abstract: https://pubmed.ncbi.nlm.nih.gov/31806905/
- Franceschi, C., Capri, M., Monti, D., Giunta, S., Olivieri, F., Sevini, F., Panourgia, M. P., Invidia, L., Celani, L., Scurti, M., Cevenini, E., Castellani, G. C., & Salvioli, S. (2007). Inflammaging and anti-inflammaging: a systemic perspective on aging and longevity emerged from studies in humans. Mech Ageing Dev, 128(1), 92–105. Abstract: https://pubmed.ncbi.nlm.nih.gov/17116321/
- Prattichizzo, F., Bonafè, M., Ceka, A., Giuliani, A., Rippo, M. R., Re, M., Antonicelli, R., Procopio, A. D., & Olivieri, F. (2016). Endothelial Cell Senescence and Inflammaging: MicroRNAs as Biomarkers and Innovative Therapeutic Tools. Current drug targets, 17(4), 388–397. Abstract: https://pubmed.ncbi.nlm.nih.gov/26240055/
- Zelová, H., & Hošek, J. (2013). TNF-α signalling and inflammation: interactions between old acquaintances. Inflammation research: official journal of the European Histamine Research Society, 62(7), 641–651. Abstract: https://pubmed.ncbi.nlm.nih.gov/23685857/
- Salvioli S., Capri, M., Valensin, S., Tieri, P., Monti, D., Ottaviani, E., & Franceschi, C. (2006). Inflamm-aging, cytokines and aging: state of the art, new hypotheses on the role of mitochondria and new perspectives from systems biology. Current pharmaceutical design, 12(24), 3161–3171. Abstract: https://pubmed.ncbi.nlm.nih.gov/16918441/
- Chen, G., & Yung, R. (2019). Meta-inflammaging at the crossroad of geroscience. Aging medicine, 2(3), 157–161. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6880720/
- Bartlett, D. B., Firth, C. M., Phillips, A. C., Moss, P., Baylis, D., Syddall, H., Sayer, A. A., Cooper, C., & Lord, J. M. (2012). The age-related increase in low-grade systemic inflammation (Inflammaging) is not driven by cytomegalovirus infection. Aging cell, 11(5), 912–915. Abstract: https://pubmed.ncbi.nlm.nih.gov/22708923/
- Shintouo, C. M., Mets, T., Beckwee, D., Bautmans, I., Ghogomu, S. M., Souopgui, J., Leemans, L., Meriki, H. D., & Njemini, R. (2020). Is inflammageing influenced by the microbiota in the aged gut? A systematic review. Exp gerontol, 141, 111079. Abstract: https://pubmed.ncbi.nlm.nih.gov/32882334/
- Velissaris, D., Pantzaris, N., Koniari, I., Koutsogiannis, N., Karamouzos, V., Kotroni, I., Skroumpelou, A., & Ellul, J. (2017). C-Reactive Protein and Frailty in the Elderly: A Literature Review. Journal of clinical medicine research, 9(6), 461–465. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5412518/
- Xia, S., Zhang, X., Zheng, S., Khanabdali, R., Kalionis, B., Wu, J., Wan, W., & Tai, X. (2016). An Update on Inflamm-Aging: Mechanisms, Prevention, and Treatment. Journal of immunol research, 2016, 8426874. Abstract: https://pubmed.ncbi.nlm.nih.gov/27493973/
- Frasca, D., & Blomberg, B. B. (2016). Inflammaging decreases adaptive and innate immune responses in mice and humans. Biogerontology, 17(1), 7–19. Abstract: https://pubmed.ncbi.nlm.nih.gov/25921609/
- Guimarães, G. R., Almeida, P. P., de Oliveira Santos, L., Rodrigues, L. P., de Carvalho, J. L., & Boroni, M. (2021). Hallmarks of Aging in Macrophages: Consequences to Skin Inflammaging. Cells, 10(6), 1323. Abstract: https://pubmed.ncbi.nlm.nih.gov/34073434/
- Nilsson, M. I., Bourgeois, J. M., Nederveen, J. P., Leite, M. R., Hettinga, B. P., Bujak, A. L., May, L., Lin, E., Crozier, M., Rusiecki, D. R., Moffatt, C., Azzopardi, P., Young, J., Yang, Y., Nguyen, J., Adler, E., Lan, L., & Tarnopolsky, M. A. (2019). Lifelong aerobic exercise protects against inflammaging and cancer. PloS one, 14(1), e0210863. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6347267/
- Walker, E. M., Slisarenko, N., Gerrets, G. L., Kissinger, P. J., Didier, E. S., Kuroda, M. J., Veazey, R. S., Jazwinski, S. M., & Rout, N. (2019). Inflammaging phenotype in rhesus macaques is associated with a decline in epithelial barrier-protective functions and increased pro-inflammatory function in CD161-expressing cells. GeroScience, 41(6), 739–757. Abstract: https://pubmed.ncbi.nlm.nih.gov/31713098/
- Liu, Y. Z., Wang, Y. X., & Jiang, C. L. (2017). Inflammation: The Common Pathway of Stress-Related Diseases. Frontiers in human neuroscience, 11, 316. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5476783/
- Mullington, J. M., Simpson, N. S., Meier-Ewert, H. K., & Haack, M. (2010). Sleep loss and inflammation. Best practice & research. Clinical endocrinology & metabolism, 24(5), 775–784. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3548567/