Acne
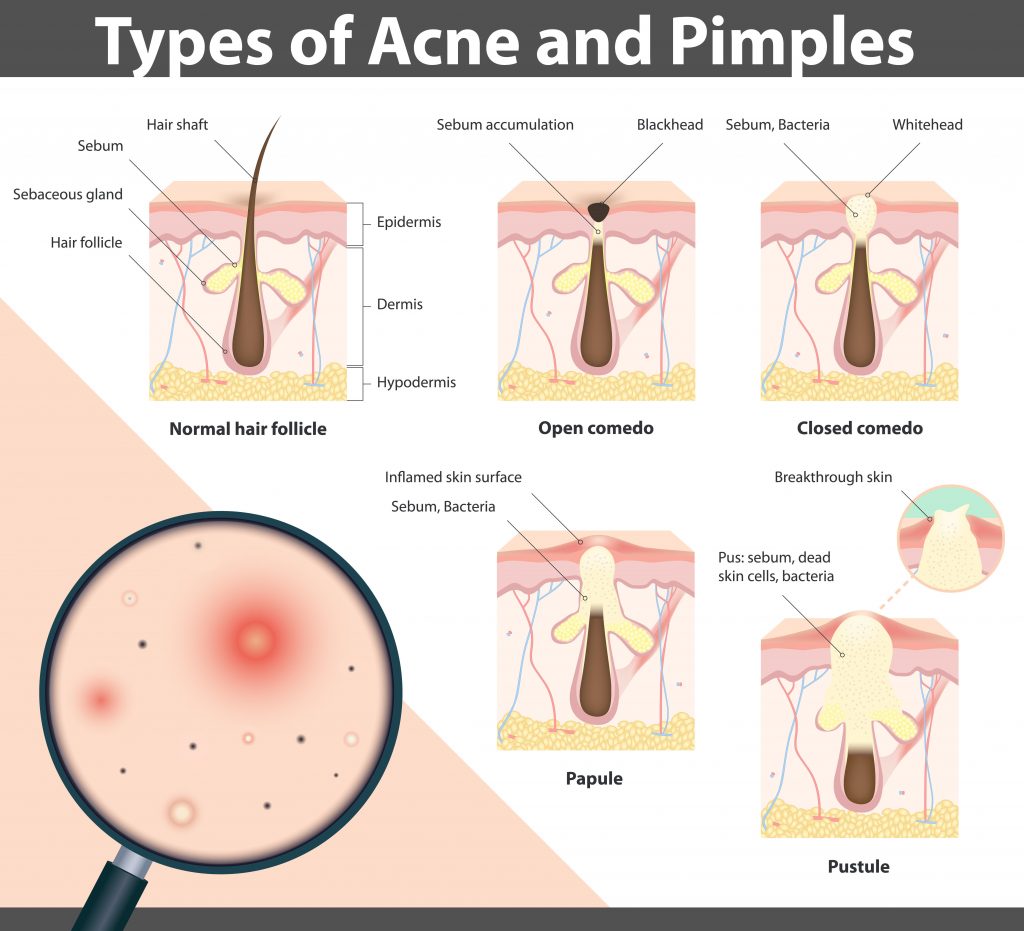
Acne is the most common skin condition in the United States. To first understand acne, we will review the components of a pilosebaceous unit. A pilosebacous unit consists of a pore opening, hair root and bulb, and a sebaceous (oil) gland and duct. The oil from the sebaceous gland is called sebum and it’s the skin’s natural oil to help keep the skin supple and healthy. Normally, sebum is excreted from the gland into the pore and dead skin cells shed into the pore as well. The sebum and dead skin cells emerge onto the skin surface at the pore’s opening.
When the sebaceous gland or duct becomes blocked with a combination of sebum and dead skin cells, they build up and it forms a hard plug that blocks the pore from opening. This leads to whiteheads and blackheads.
A whitehead is called a “closed comedone” and it is when the oil gland is filled with sebum and dead skin cells, but the opening to the surface of the skin is still covered.
A blackhead is also called an “open comedone” and it is when an oil gland that is filled with sebum and dead skin cells is open to the surface, which forms a black appearing spot on the skin.
When whiteheads and blackheads occur, it provides a favorable environment for some changes in the microbiome of the skin. In these conditions, a bacteria called Propionibacterium acnes (P. acnes) that is normally found on the skin, begins to grow out of control. When there is an overgrowth of P. acnes, white blood cells rush to fight the overgrowth and the skin swells and this leads to inflammatory acne lesions. Inflammatory pustules and papules develop when there is inflammation, redness and swelling of the clogged pore.
When inflammatory papules are deeper and are mostly under the surface of the skin they are considered cysts and large cysts are referred to nodules.
Treatment Options
The type of acne lesions you have guides your treatment options. Please see your integrative dermatologist to discuss what treatment modalities fit best for you.
Aging & Benign Growths
Over time our skin cells degenerate and decreases in the firmness and elasticity of the skin are noted. We also acquire discolored spots on our skin. We will discuss briefly three common growths that we acquire on our skin with more birthdays: solar lentigos, seborrheic keratoses, and angiomas.
Solar Lentigos
Solar lentigos are tan, brown or dark black flat spots on sun exposed areas of the body such as face, neck, chest, ears, arms, hands and back. Sometimes they are round or oval in appearance, but they can also be irregularly shaped. Their prevalence is more common in lighter skin types and their incidence increases with advancing age with many people having them by age 60. Some people when they have them on the back of their hands refer to them as liver spots.
Solar lentigos are due to an accumulation of melanin in skin cells in response to chronic sun exposure.
It is possible for a lentigos to have malignant changes called a lentigo maligna.
Yes! An irregular brown spot on your skin should always be evaluated by your dermatologist.
Most people leave these alone. Treatment options include liquid nitrogen and laser.
Seborrheic Keratosis
Seborrheic keratoses are incredibly common. Their appearance is rather variable, however, classically they are brown stuck on bumps with rough, bumpy texture. Frequently, it looks like you could just scratch them off with your fingernail. But we advise you don’t as they will bleed and you will risk an infection from having the open wound. Seborrheic keratosis can also be all shades of brown, tan, pink, skin-colored, white, black and even have multiple within one lesion. Their size varies from a tiny pinpoint bump to a large plaque measuring several centimeters. They can grow and enlarge, however, not all of them do. They occur only on areas of our skin that we have hair and do not occur on palms and soles or mouth. Most of us have them by our 40’s and we continue to acquire them as we advance through life. I have a special name for these because of that reason. I call them “Wisdom Spots”.
The cause of seborrheic keratoses is unknown.
No. They are benign. However, you can get a skin cancer next to a seborrheic keratosis. So if any of your spots change, make an appointment to see your dermatologist.
Sometimes they can become irritated or itchy and even bleed. They can also get caught on clothing, jewelry, etc. Sometimes they can become infected.
They are benign and healthy growths and can be challenging to get rid of so many people opt to just keep them. Treatments do not prevent new ones from occurring and sometimes the lesions return after treatment. They can be treated with cryotherapy, CO2 or erbium:YAG lasers, cautery.
Cherry Angioma
These are those red dots that appear out of nowhere on your skin. Most common locations are on the abdomen, but they can occur anywhere on the body. They vary in size from tiny pinpoint spots to large red and sometimes purple / black spots.
It is not known at this time.
Yes, when they are deeper under the skin they can appear almost black. They can then be confused with a black mole that can sometimes be melanoma. Sometimes melanoma can be a red spot so if you have a red or black spot you aren’t sure about, have it evaluated!
Most people opt to leave these alone as they are most commonly in areas where skin is covered by clothing. Most common treatment options are to destroy them with electrocautery or with pulsed dye laser.
Atopic Dermatitis
AD is a complex skin disease and at this time there is not a way to detect if it will go away or be a lifelong issue. However, it does tend to improve with age. If you have atopic dermatitis, you may be more prone to develop skin allergies and contact or irritant dermatitis. Therefore, it is recommended that if you are prone to AD that you select skin care products that are fragrance-free and avoid perfumes or scented products. Sometimes finding the products that work best for you may be “trial and error” sampling of different products until you find one that works for you.
One of the important components to improving AD is moisturizing your skin. Consider your moisturizer as a barrier to help soothe and seal dry, scaling skin. Another tip is to avoid any triggers that tend to make your AD worse.
Discuss skin care and comprehensive treatment options with your integrative dermatologist for your individualized treatment plan.
Cold Sores
Cold sores are caused by a virus called herpes simplex. There is more than one strain of herpes simplex virus (HSV) and most cold sores are caused by HSV-1. Genital herpes is more commonly caused by HSV-2, however either strain can cause a sore on the face or genitalia. After exposure to this virus you may have no reaction or a very severe reaction with blisters. Some experience a tingling, itchy or burning sensation before the skin sore appears. They can be painful and sore and develop into blisters. The sores can last up to 7-10 days. Some people also experience flu-like symptoms.
HSV is contagious and can spread with skin-to-skin contact. It is not necessary to have the sore to spread the virus as people that can shed the virus in their skin cells without knowing it. This is called “asymptomatic viral shedding”. Once exposed to this virus it stays with you and remains dormant in our nervous system forever. It can be triggered to become active again. These triggers make the virus active and HSV travels out along a nerve ending and then forms the sore on our skin. Because it lives in the nerve ending, many people can feel a cold sore before it starts. Some of these triggers may be heat, friction, sun exposure, stress, fatigue, trauma, illness, surgery, hot foods and spicy foods.
Avoiding triggers is key to preventing a cold sore. Eating healthy and keeping stress levels low also can help prevent a break out. When you first notice the sensation of a cold sore is the best time to start treating. There are over-the-counter as well as prescription treatment options for cold sores. Be sure to discuss strategies to improve your overall health, immunity and ways to handle stress with your integrative physician.
Contact/Irritant Dermatitis
Contact dermatitis is when something that touches your skin gives you an allergic itchy rash. In the majority of cases, the cause of the rash can be difficult to determine, as the rash doesn’t necessarily appear the first time you are exposed to it. More commonly, it is a rash from an item that you have used repeatedly. Irritant dermatitis is when the skin is injured by environmental factors such as water or chemicals faster than the skin can repair itself. Typically, irritants remove the natural moisturizing factor and oils from our skin, which decreases the barrier of the skin and allows chemicals to cause more damage and trigger more inflammation. Anyone can get irritant dermatitis or contact dermatitis, although if you have atopic dermatitis you are more likely.
The keys to healing contact/irritant dermatitis is avoiding the cause of the rash, using thick moisturizing creams to help seal the barrier of the skin and using gentle skin care techniques. Treatment modalities will depend on the part(s) of the body involved with the rash, the severity of the rash, the length of time you have had it and likelihood of re-exposure and recurrence of the rash. Sometimes it can be challenging to determine what item(s) triggered your rash and you may explore allergy testing.
If you are prone to contact/irritant dermatitis, keep your skin care products simple and as chemical-free as possible, eat healthy and remember gentle skin care. Discuss your comprehensive, individualized treatment plan with your integrative dermatologist.
Moles
Moles are very common. They are also referred to as nevi if there is more than one and nevus when referring to one mole. Moles come from the cells called melanocytes that are in the epidermis. Most of the time, moles are benign, however they do have the potential to turn into a skin cancer called melanoma.
One guideline to determine whether a mole is worrisome for possible melanoma is to see if it fits into the ABCDE parameters. If you ever are not sure whether your mole is normal or not, please see your dermatologist for evaluation. Here is a summary of what the ABCDE’s represent.

If you have any change in your mole, seek an appointment with your dermatologist immediately. Knowing what your moles normally look like and recognizing when they change could save your life.
Psoriasis
Psoriasis is a chronic skin condition that leads to the growth of new skin cells. This leads to developing new skin cells in a matter of days rather than weeks. The build up of these new skin cells do not shed and instead pile up forming areas of red, scaling skin.
Researchers are still trying to understand what causes psoriasis. Currently, it is thought that the immune system sends a signal that tells the skin to make more cells too fast. Researchers have also found that psoriasis has a genetic component as it occurs more commonly in individuals that have another family member with psoriasis. It is not contagious. Psoriasis can occur any part of the body, but the most common areas affected are elbows, knees, scalp, and groin. Joints can also be affected and this is referred to as psoriatic arthritis. Sometimes things like a stressful event, strep throat, medications, injury/trauma to skin can trigger psoriasis.
Recently, psoriasis has been recognized as a systemic (whole body) disease relating to inflammation. Psoriasis patients have a higher risk of developing metabolic syndrome (obesity, diabetes, high blood pressure and high cholesterol) and heart disease. Therefore, eating a healthy diet and balancing stress are just as important as sticking to your skin care regimen when managing your psoriasis.
There are many comprehensive treatment options for psoriasis. Meet with your integrative dermatologist to discuss your individualized treatment plan.
Rosacea
Rosacea is a common skin issue and more than 14 million people have rosacea. It can vary from redness on the face with flushing, to red pimple breakouts, to dryness of the eyes and even thickness of the skin (nose most commonly).

Researchers don’t know what causes rosacea, however they have discovered some information. Rosacea is more common if other family members also have rosacea. Scientists also have found that the immune system is a key factor in rosacea. There are several theories that an overgrowth of certain bacteria on the skin (ex. Bacillus oleronis), a mite that lives on everyone’s skin (Demodex) or a bacterial overgrowth in the gastrointestinal system (ex. H. pylori). It is thought that rosacea may be a result of a dysregulation of the immune system response to these factors or a dysfunction in the immune system that leads to the overgrowth. However, not all people that have rosacea have been found to have these issues.
Stress, sunlight, foods or beverages can trigger rosacea. Avoiding your triggers can be helpful in preventing breakouts or flares of your rosacea. Additionally, practicing gentle skin care, avoiding harsh cosmetic products, protecting your skin with sunscreen and using an emollient to help repair the skin can also help your rosacea breakouts. A comprehensive integrative treatment regimen for rosacea includes nutrition and dietary changes, avoiding triggers, developing consistent strategies to mange stress as well as topical and sometimes oral medications. Lasers and other light treatments can be used to treat redness.
Skin Cancer
Skin cancer occurs when there is an overgrowth of a certain cell type that makes up the skin. There are several types of skin cancer with the most common being pre-skin cancers or actinic keratoses, basal call carcinoma, squamous cell carcinoma and melanoma. Other more rare types of skin cancers may also occur such as merkel cell, cutaneous t-cell lymphoma, etc.
A pre-skin cancer is when a cluster of atypical cells is just sitting on the surface of the skin and we refer to them as actinic keratoses. Approximately 1-10% of these have the potential to develop into skin cancers. They can be easily treated by your dermatologist with various modalities including, but not limited to, liquid nitrogen, photodynamic therapy, topical imiquimod, topical 5-flurouracil.
A basal cell carcinoma (BCC) is an overgrowth of the cells that make up the basal layer of the epidermis. BCC has various subtypes depending on it’s growth pattern. It may be superifical creating a pink scaling spot on the surface of the skin, or it may be nodular or microdoular forming collections of the skin cancer cells in the skin of various sizes. It may also be sclerosing or infiltrative where it forms scars and has finger –like projections that dive into the skin. Treatment options for BCC depend on the subtype, size and location of the skin cancer. Treatment modalities range from topical imiquimod, electrodessication & curettage, excision or Mohs Micrographic Surgery. If left untreated, these do not typically resolve on their own and continue to destroy skin and tissue and can develop ulcers or sores in them that bleed. They also have the potential to break off and spread or metastasize, although this is not as common.
A squamous cell carcinoma (SCC) is made of cells that make up the skin called squamous cells. The squamous cell is a type of cell that is also found in other tissues such as the lining of the lung, etc. SCC in skin behaves much differently than SCC in the lung or other organs. A squamous cell carcinoma that just is sitting on the top layer of the skin (epidermis) is called a SCC in situ. These can be treated with electrodessication and curettage. If they have become more invasive or travel down a hair follicle then excision or Mohs Micrographic surgery is indicated. Some SCC’s can be more aggressive and can invade the nerve (perineural invasion) and may break off and metastasize.
A melanoma is when a mole made of melanocytes has become cancerous. These can also just be located in the very top layer of the skin (epidermis) and are referred to as melanoma in situ. When melanoma is caught in this early stage, it has the highest cure rate. When it progresses deeper into the skin the risk of metastasizing greatly increases. When a melanoma is more than 1mm in depth and sometimes 0.76mm in depth, the suspicion for metastases increases and a sentinel lymph node biopsy is performed. Your dermatologist and/or oncologist may also advise further evaluation for metastatic melanoma.
Warts
Warts appear as bumps on the skin and they may be skin-colored, brown, or gray-black. Sometimes they are raised and other times are somewhat flat. If you look closely, you may notice little black dots in them, which represent tiny blood vessels located within the wart.
Warts can grow on any part of your body and are contagious because a virus called the Human Papillomavirus (HPV) causes them. Anyone can get warts and some people are more prone to getting them than others. There are over 60 strains of HPV.
Warts commonly occur in areas of broken or injured skin and can be spread to others areas of the body by scratching or picking at the wart. Many times warts resolve without any treatment, especially in children.
Over-the-counter and in-office treatments of warts are challenging as it almost always takes time and multiple repeated treatments. If you suspect that you have warts, talk with your integrative dermatologist to discuss over-the-counter topical and oral treatments/supplements as well as in-office procedures.
Sometimes warts can mimic skin cancer so be sure to have any new or suspicious growth evaluated by your dermatologist.
